Our Courses
Provide a general summary of the services you provide, highlighting key features and benefits for potential clients.


What is Medical Coding?
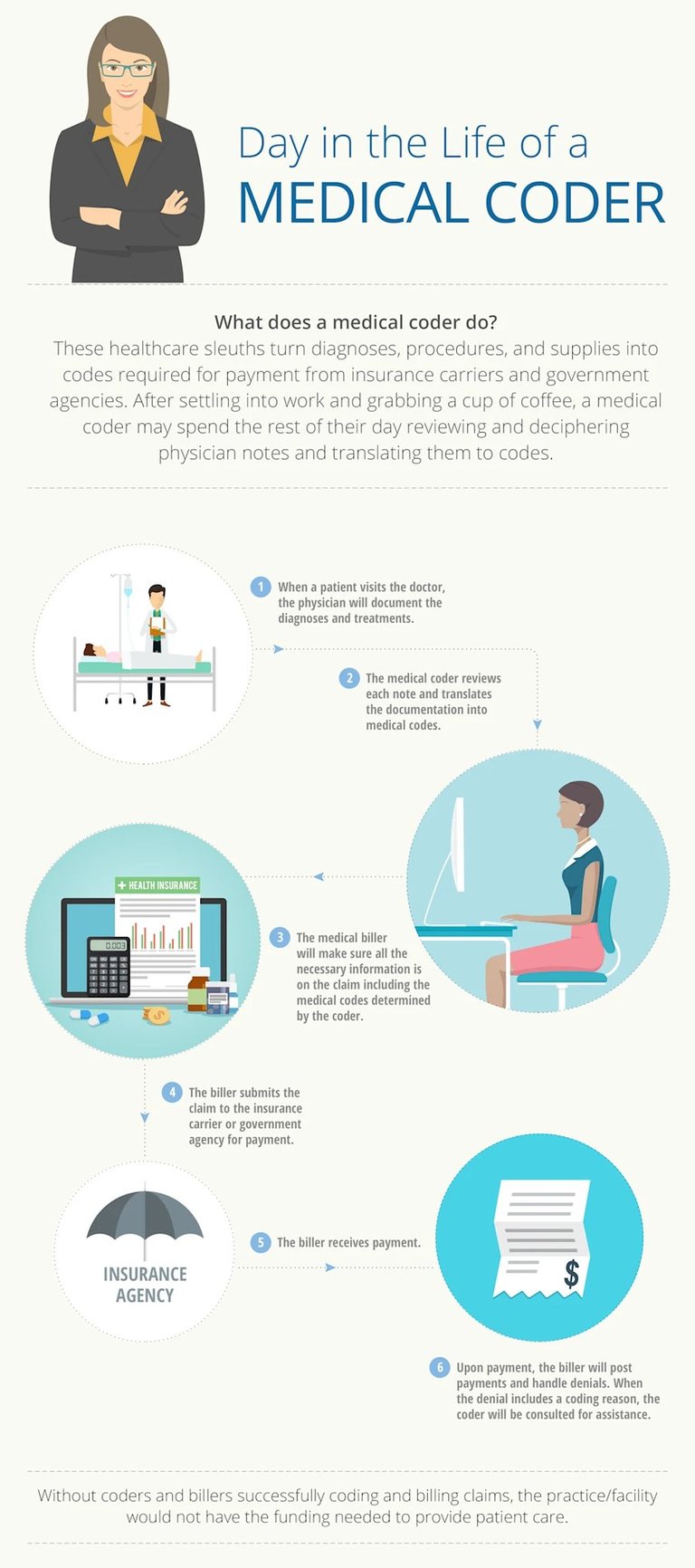
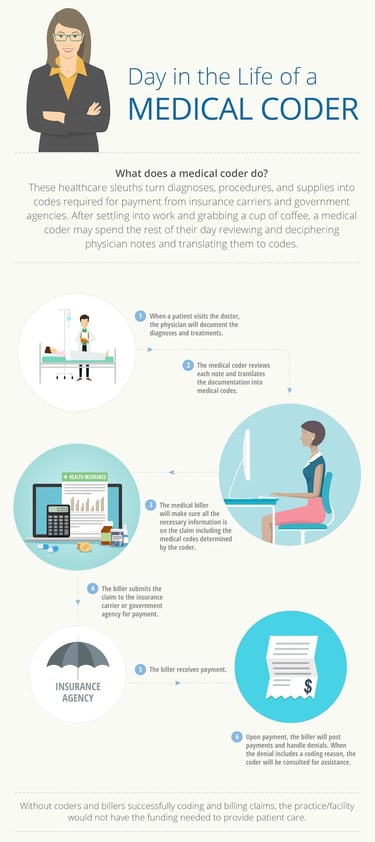
Medical coding is the transformation of healthcare diagnosis, procedures, medical services, and equipment into universal medical alphanumeric codes. The diagnoses and procedure codes are taken from medical record documentation, such as transcription of physician's notes, laboratory and radiologic results, etc.
Medical coding professionals help ensure the codes are applied correctly during the medical billing process, which includes abstracting the information from documentation, assigning the appropriate codes, and creating a claim to be paid by insurance carriers.
Medical coding happens almost every time you see a healthcare provider. The healthcare provider reviews your complaint and medical history, makes an expert assessment of what’s wrong and how to treat you, and documents your visit. That documentation is not only the patient’s ongoing record, it’s how the healthcare provider gets paid.
What you will learn?
Medical Terminology
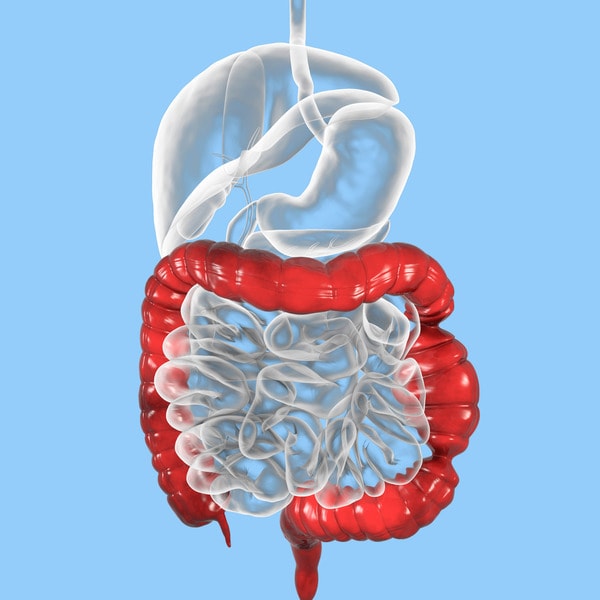
Human Anatomy & Physiology
Pathophysiology
About Course
Medical coders translate documentation into standardized codes that tell payers the following:
Patient's diagnosis
Medical necessity for treatments, services, or supplies the patient received
Treatments, services, and supplies provided to the patient
Any unusual circumstances or medical condition that affected those treatments and services
Medical Coding
Why is medical coding needed?
A patient's diagnosis, test results, and treatment must be documented, not only for reimbursement but to guarantee high quality care in future visits. A patient's personal health information follows them through subsequent complaints and treatments, and they must be easily understood. This is especially important considering the hundreds of millions of visits, procedures, and hospitalizations annually in the United States.
The challenge, however, is that there are thousands of conditions, diseases, injuries, and causes of death. There are also thousands of services performed by providers and an equal number of injectable drugs and supplies to be tracked. Medical coding classifies these for easier reporting and tracking. And in healthcare, there are multiple descriptions, acronyms, names, and eponyms for each disease, procedure, and tool. Medical coding standardizes the language and presentation of all these elements so they can be more easily understood, tracked, and modified.
This common language, mandated by the Health Information Portability and Accountability Act (HIPAA), allows hospitals, providers, and payers to communicate easily and consistently. Nearly all private health information is kept digitally and rests on the codes being assigned.
Types of codes used
ICD-10-CM (International Classification of Diseases, 10th Edition, Clinically Modified)
ICD-10-CM includes codes for anything that can make you sick, hurt you, or kill you. The code set is made up of more than 70,000 codes for conditions and diseases, poisons, neoplasms, injuries, causes of injuries, and activities being performed when the injuries were incurred. Codes are “smart codes” of up to seven alphanumeric characters that specifically describe the patient’s complaint.
ICD-10-CM is used to establish medical necessity for services and for tracking. It also makes up the foundation of the MS-DRG system below.
CPT® (Current Procedure Terminology)
This code set, owned and maintained by the American Medical Association, includes more than 11,000 five-character numeric and alphanumeric codes describing services provided to patients by physicians, paraprofessionals, therapists, and others. Most outpatient services are reported using the CPT® system. Physicians also use it to report services they perform in inpatient facilities. Here's a little behind the scenes on the making of CPT® codes.
ICD-10-PCS (International Classification of Diseases, 10th Edition, Procedural Coding System)
ICD-10-PCS is a 75,000+ alphanumeric code set used by hospitals to describe surgical procedures performed in operating, emergency department, and other settings. Don’t let the procedural coding intimidate you by taking the right approach to ICD-10-PCS coding.
HCPCS Level II (Health Care Procedural Coding System, Level II)
Developed originally for use by Medicare, Medicaid, Blue Cross/Blue Shield, and other providers to report procedures and bill for supplies, HCPCS Level II’s 7,000+ alphanumeric codes are used for many more purposes, such as quality measure tracking, outpatient surgery billing, and academic studies.
CDT® (Code on Dental Procedures and Nomenclature)
CDT® codes are owned and maintained by the American Dental Association (ADA). The five-character codes start with the letter D and used to be the dental section of HCPCS Level II. Most dental and oral procedures are billed using CDT® codes.
NDC (National Drug Codes)
The NDC code set is used to track and report all packages of drugs. The 10-13 alphanumeric character smart codes allow providers, suppliers, and federal agencies to identify drugs prescribed, sold, and used.
Modifiers
CPT® and HCPCS Level II codes use hundreds of numeric and alphanumeric two-character modifier codes to add clarity to coding. Modifiers may indicate the status of the patient, the part of the body on which a service is being performed, a payment instruction, an occurrence that changed the service the code describes, or a quality element.
MS-DRG and APC
Two federal code sets used to facilitate payment deriving from those above systems are MS-DRG and APCs. They rely on existing codes sets but indicate the resources consumed by the facility to perform the service.
MS-DRG (Medical Severity Diagnosis Related Groups)
MS-DRGs are reported by a hospital to be reimbursed for a patient’s stay. The MS-DRG is based on the ICD-10-CM and ICD-10-PCS codes reported. They are defined by a particular set of patient attributes which include principal diagnosis, specific secondary diagnoses, procedures, sex, and discharge status. The Centers for Medicare & Medicaid Services (CMS) work with 3M HIS to maintain this data set.
APC (Ambulatory Payment Categories)
APCs are maintained by the Centers for Medicare & Medicaid Services (CMS) to support the Hospital Outpatient Prospective Payment System (OPPS). Some outpatient services in a hospital, such as minor surgery and other treatments, are reimbursed through this system.
How do you become a medical coder?
Successful medical coders know anatomy, physiology, medical procedures, and payer rules and policies. To become a medical coder, you must attend training via a coding-specific training program or college. Afterward, finding a job in the field is easier if you have a professional credential, such as AAPC's or AHIMA.
There are several medical coding certifications available, depending on the area of the revenue cycle you wish to pursue. The baseline for most is the Certified Professional Coder (CPC), which certifies the coder’s ability to work in outpatient settings. Facility coders should pursue the Certified Inpatient Coder (CIC) for inpatient coding and Certified Outpatient Coder (COC) for hospital patients receiving in-and-out services. Here’s an infographic to help you choose the right hospital credential. There are several programs available both for online training on medical coding and physical medical coding training classes.
Today more than 250,000 medical professionals are members of AAPC. AAPC elevates the standards of medical coding by developing training, professional certification, opportunities to network with other related medical professionals and providing a variety of job search and career building opportunities.
Professional coders largely work independently. However, interaction with coding staff, medical billers, physicians, and ancillary office staff is essential. Medical coders are usually placed on tight production schedules and expected to complete a determined number of notes each day or to keep their lag days at a specified timeframe. Lag days are the number of days it takes for the notes to be documented to the actual claims submission date. The prime date is usually between two to five days.
Depending on the clinical setting, internal or external auditors periodically perform audits of the coding and documentation for accuracy and completeness. The results of these coding audits are maintained by the compliance department or the department supervisor and are a significant part of job evaluations.
Study about structure and functions.
Anatomy & Physiology
Medical Terminology
ICD-10-CM/CPT/HCPCS/PCS
Language of Medicine
Coding Subjects.
Medical Terminology
Medical terminology is the language of healthcare. It’s the means for healthcare professionals to confer on the intricacies of the human body, both in states of health and states of injury or disease. As such, medical terminology comprises the lexicon of labels for all known anatomical features, physiological processes, and medical interventions.


Medical Prefixes: When included, the prefix appears at the beginning of a medical term and usually indicates location, direction, time, quality, or quantity.
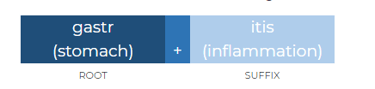
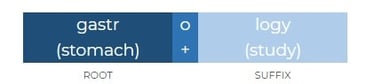
Medical Suffixes: The suffix is tacked onto the end of a term and typically indicates a procedure, function, test, condition, or pathology. The suffix may also identify if the term is a noun, adjective, or verb.
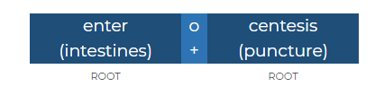
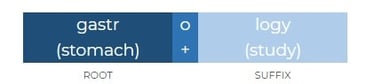
Medical Root Words: The root word is the base part of the medical term and conveys its primary meaning, which is often a body part or body system. Most medical terms contain one or more root words.
3 component types
Medical terms to their components
Prefix, root word, suffix
Root word, suffix
Root word, root word, suffix
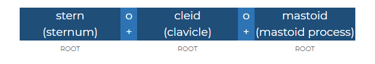
Root word, root word, root word
Medical terminology often combines root words, prefixes, and suffixes to describe conditions, procedures, or anatomy. Here are some examples:
Root Words:
Cardi: Refers to the heart (e.g., cardiology - study of the heart).
Derm: Refers to the skin (e.g., dermatology - study of the skin).
Neuro: Refers to nerves (e.g., neurology - study of the nervous system).
Suffixes:
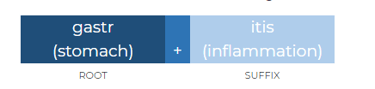
-itis: Indicates inflammation (e.g., arthritis - inflammation of the joints).
-ectomy: Refers to surgical removal (e.g., appendectomy - removal of the appendix).
-logy: Refers to the study of something (e.g., biology - study of life).
Root word + Suffix
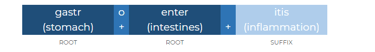
Root word + Root word + Suffix
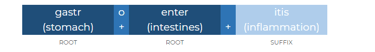
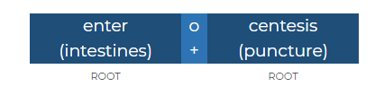
In medical terminology, combining two root words with a suffix is common to describe complex conditions or anatomical structures. Here are some examples:
Gastroenterology:
Gastro (stomach) + Entero (intestine) + -logy (study of) = Study of the stomach and intestines.
Cardiomyopathy:
Cardio (heart) + Myo (muscle) + -pathy (disease) = Disease of the heart muscle.
Osteoarthritis:
Osteo (bone) + Arthro (joint) + -itis (inflammation) = Inflammation of the bone and joint.
Root word + Root word + Suffix
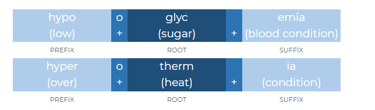
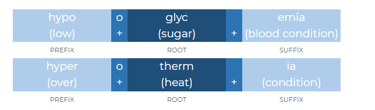
Here are some examples of medical terms that combine a prefix, root word, and suffix:
Hypertension:
Hyper (prefix, meaning excessive) + Tens (root word, meaning pressure) + -ion (suffix, meaning condition) = Condition of excessive pressure.
Hypoglycemia:
Hypo (prefix, meaning below) + Glyc (root word, meaning sugar) + -emia (suffix, meaning blood condition) = Low blood sugar condition.
Endocarditis:
Endo (prefix, meaning within) + Card (root word, meaning heart) + -itis (suffix, meaning inflammation) = Inflammation within the heart.
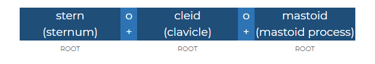
Root word + Root word + Root word
Sternocleidomastoid. In this example, three root words are combined to form sternocleidomastoid, which refers to a muscle on each side of your neck that starts at the top of the sternum and the clavicle, then reaches up to insert behind your ear on the mastoid process of the temporal bone.
It’s an unusual medical term, in that it doesn’t have a suffix. As you’ll soon see, though, -oid is a suffix meaning to resemble or similar to. Because it’s built into the root word mastoid, these three root words together are complete.
Stern(o) + cleid(o) + mastoid Sternum+clavicle+mastoid process
The term "sternocleidomastoid" refers to a muscle in the neck, and its name is derived from its anatomical attachments:
Sterno: Refers to the sternum (breastbone), where one part of the muscle originates.
Cleido: Refers to the clavicle (collarbone), which is another point of origin for the muscle.
Mastoid: Refers to the mastoid process of the temporal bone, where the muscle inserts.
This muscle plays a key role in head and neck movement, including rotation and flexion.






Quick links
Contact Us
+91 - 80720 20716
medicalcodingofficers@gmail.com
All Rights Reserved. Website Design by Medical Coding Officers Academy
Medical Coding Officers Academy
India's top most training center for medical coding, billing and RCM in healthcare industry.
Subscribe to our newsletter
70/1, 2nd Floor, 200 Feet Radial Road, Pallavaram to Thuraipakkam Road, Near A2B Restaurant, Pallikaranai, Chennai, Tamil Nadu 600100