Certified Professional Coder (CPC)® Online/Classroom Training Course
CPC® Exam Review
Learn testing strategies
Review frequently missed questions
Participate in a focused review of each domain of the exam
Review sample test questions to solidify learning as you progress through the review


International Certification Preparation Training on
Identify the purpose of the CPT® , ICD-10-CM, and HCPCS Level II code books
Understand and apply the official ICD-10-CM coding guidelines
Apply coding conventions when assigning diagnoses and procedure codes
Identify the information in appendices of the CPT® code book
Explain the determination of the levels of E/M services
Code a wide variety of patient services using CPT® , ICD-10-CM, and HCPCS Level II codes
List the major features of HCPCS Level II codes
Provide practical application of coding operative reports and evaluation and management services
Course Objective:
The Business of Medicine
Review of Anatomy
Overview of ICD-10-CM
Applying the ICD-10-CM Guidelines
Accurate ICD-10-CM Coding
Introduction to CPT®, HCPCS Level II, and Modifiers
Integumentary System
Musculoskeletal System
Respiratory System
Cardiovascular System
Hemic & Lymphatic Systems, Mediastinum, Diaphragm
Digestive System
Urinary System and Male Genital System
Female Reproductive System and Maternity Care & Delivery
Endocrine System and Nervous System
Special Senses (Ocular and Auditory)
Anesthesia
Radiology
Pathology & Laboratory
Evaluation & Management Services
Medicine
Methods of Evaluation:
Successful course completion includes:
An attempt of all required assignments
A passing score of 70% or higher on all chapter exams
A passing score of 70% or higher on the final exam
An overall final course score of 70% or higher No reduced hours in the course or tuition discount for previous education or training will be granted.
Required Code Books:
CPT® Professional Edition code book (current year), AMA publisher
ICD-10-CM code book (current year), any publisher
HCPCS Level II code book (current year), any publisher

Course Content:
Certified Coding Specialist (CCS®)
The Certified Coding Specialist certification is designed for individuals skilled in classifying medical data from medical records. CCS professionals demonstrate a practitioner’s tested skills in data quality and accuracy as well as mastery of coding proficiency.


International Certification Preparation Training on
Domain 1 – Coding Knowledge and Skills (39-41%)
It is recommended, not required, to have at least one of the following:
Complete courses in all the following topics: anatomy & physiology, pathophysiology, pharmacology, medical terminology, reimbursement methodology, intermediate/advanced ICD diagnostic coding, and procedural coding and medical services (CPT/HCPCS) plus one (1) year of coding experience directly applying codes; OR
Minimum of two (2) years of related coding experience directly applying codes; OR
Hold the CCA® credential plus one (1) year of coding experience directly applying codes; OR
Hold a coding credential from another certifying organization plus one (1) year of coding experience directly applying codes; OR
Hold a CCS-P®, RHIT®, or RHIA® credential
Prepare for the exam
Required Code Books:
1. Assign diagnosis and procedure codes based on the provider’s documentation in the health record
2. Identify principal/first-listed diagnosis and procedure based on the respective guidelines
3. Apply coding conventions/guidelines and regulatory guidance
4. Attach CPT/HCPCS modifiers to outpatient procedures
5. Determine appropriate sequencing of diagnoses and procedure codes based on the case scenario
6. Apply present on admission (POA) guidelines
7. Demonstrate knowledge of coding edits (e.g., NCCI, Medical Necessity)
8. Demonstrate knowledge of reimbursement methodologies (e.g., DRG, APC)
9. Abstract applicable data from the health record
10. Identify major co-morbid conditions (MCC) and co-morbid conditions (CC)
CPT® Professional Edition code book (current year), AMA publisher
ICD-10-CM code book (current year), any publisher
HCPCS Level II code book (current year), any publisher
Domain 2 – Coding Documentation (18-22%)
1. Resolve conflicting documentation in the health record (e.g., admission type, laterality)
2. Ensure all required documentation for assigning a specified code is available within the body of the health record
3. Verify and validate documentation within the health record
Domain 3 – Provider Queries (9-11%)
1. Resolve conflicting documentation in the health record (e.g., admission type, laterality)
2. Ensure all required documentation for assigning a specified code is available within the body of the health record
3. Verify and validate documentation within the health record
Domain 4 – Regulatory Compliance (18-22%)
1.Ensure completeness and accuracy of health records
2. Understand payer-specific guidelines
3. Identify patient safety indicators (PSIs) and hospital-acquired conditions (HACs) based on the provider’s documentation
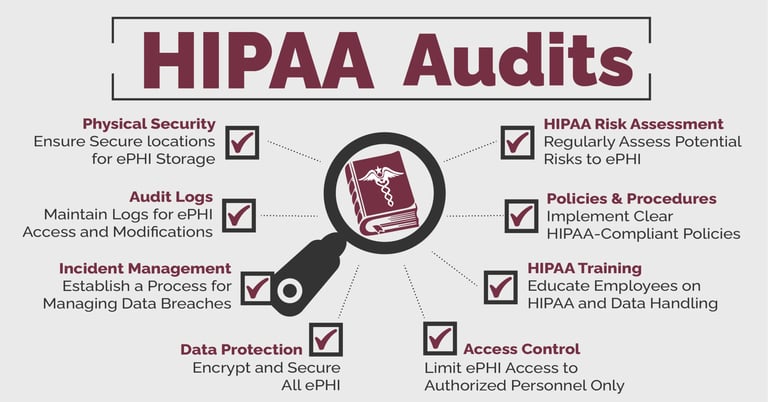
4. Ensure compliance with HIPAA guidelines
5. Ensure adherence to AHIMA Standards of Ethical Coding
6. Ensure compliance with the Uniform Hospital Discharge Data Set (UHDDS)
Domain 5 – Information Technologies (9-11%)
1.Distinguish various types of Electronic Health Records (EHR)
2. Demonstrate a basic understanding of encoding and grouper software
3. IExhibit an understanding of computer-assisted coding (CAC) software and its impact on coding
4. Ensure compliance with HITECH guidelines

Certified Professional Medical Auditor (CPMA)® certification
CPMA designed for the seasoned medical coding professional, the CPMA Training Course covers medical record standards and documentation guidelines, coding and documentation compliance, coding and reimbursement concepts, audit scope and statistical sampling methods, medical record audit abstraction, and category risk analysis and communication.
International Certification Preparation Training on
Explain the impact of the OIG Work Plan and Corporate Integrity Agreements (CIAs)
List the elements of compliance plans and identify potential compliance risk areas
Identify National Correct Coding Initiative (NCCI) and Medically Unlikely Edit (MUE) risk areas
Identify the purpose of recovery audit contractors and how to prepare for potential RAC audits · Explain the HIPAA privacy rule, including details on protected health information, minimum necessary, sharing of information, and enforcement
Identify medical record documentation standards and record retention standards
Identify common errors found in documentation for evaluation and management, anesthesia, surgery, radiology, pathology and laboratory, and medicine services
Explain the types of audits and the resources required for audits
Define steps of the audit process and identify statistical sampling types and factors
Provide practical application of auditing operative reports and evaluation and management services
Course Objective:
Compliance and Regulatory Guidelines including:
Fraud and abuse
Federal False Claims Act
Anti-Kickback Law
Stark Law
Exclusion Statute
Civil Monetary Penalties Law
Office of Inspector General (OIG)
Centers for Medicare and Medicaid Services (CMS)
Medical Record Documentation Standards
HIPAA Privacy Regulations
Types and components of medical records
Accreditation standards
Evaluation and Management Coding
Coding and Reimbursement Concepts
CPT® Guidelines
Evaluation and Management
Anesthesia
Surgery
Radiology
Pathology and Laboratory
Medicine including chemotherapy, psychotherapy, physical therapy
Modifiers o Diagnosis coding and medical necessity
Physicians at Teaching Hospital (PATH) Guidelines
Auditing
Auditing process
Statistical sampling, utilization review, RAT-STATs
Risk Analysis and Communication
Validation of audit results
Analysis and report of audit findings
Communicating audit results
Practical Expertise
Practical audit skills utilizing cases for practical application
Methods of Evaluation:
Successful course completion includes:
An attempt of all required assignments
A passing score of 70% or higher on all chapter exams
A passing score of 70% or higher on the final exam
An overall final course score of 70% or higher No reduced hours in the course or tuition discount for previous education or training will be granted.
Required Code Books:
CPT® Professional Edition code book (current year), AMA publisher
ICD-10-CM code book (current year), any publisher
HCPCS Level II code book (current year), any publisher